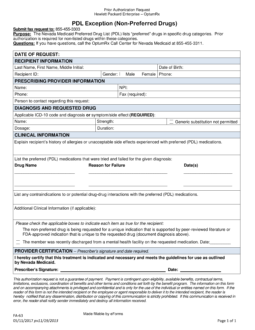
Updated July 27, 2023
A Nevada Medicaid prior authorization form requests Medicaid coverage for a non-preferred drug prescription in the state of Nevada on behalf of a certified medical practitioner. You can download a fillable PDF version of this form here. In order for your request to be eligible, you must provide a clinical justification for why you are not opting to prescribe a drug from the PDL (Preferred Drug List). Once completed, fax the prior authorization form to the fax number provided below.
Fax – 1 (855) 455-3303
Phone – 1 (855) 455-3311
Preferred Drug List – Acceptable drugs by the State