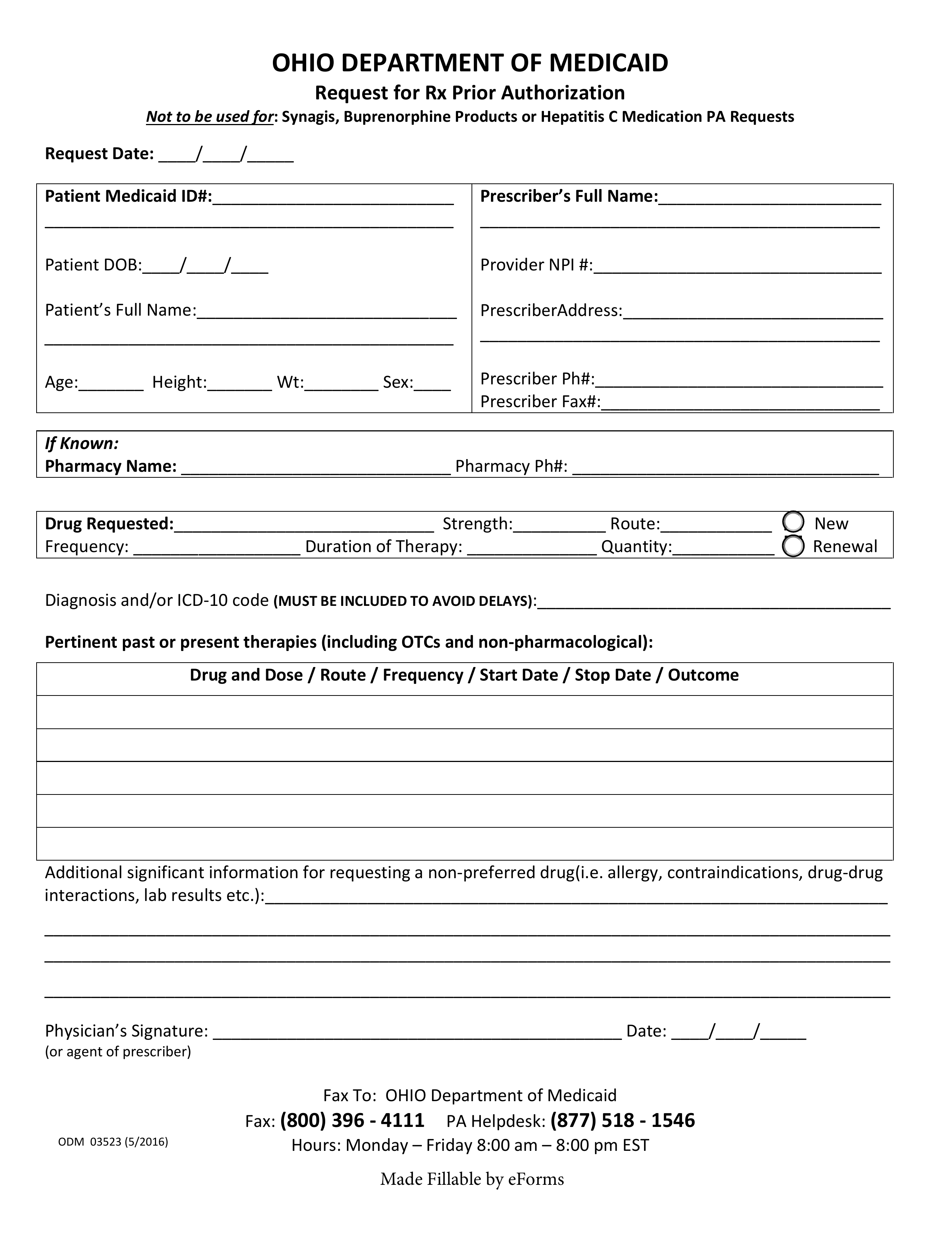
Updated July 27, 2023
An Ohio Medicaid prior authorization form is used when Ohio-based medical professionals wish to request Medicaid coverage for a non-preferred drug. A non-preferred drug is a drug that is not included on the State’s Preferred Drug List (PDL). A fillable PDF version of this form is available for download on this webpage. For more information, call the PA Helpdesk at the phone number provided below.
Fax – 1 (800) 396-4111
Phone – 1 (877) 518-1546